“POLYVAGAL THEORY” … how our NERVOUS SYSTEM “keeps the score” of our ATTACHMENT RELATIONSHIPS.
Previous blogs have covered the debilitating effects of childhood trauma and a lack of safety on an individual’s mental health and brain development. In this chapter, the focus will be on understanding how early attachment relationships, particularly loss of safety and relational disconnection have long-term effects on an individual’s nervous system and body. This area of trauma research has recently seen the emergence of many ‘body’ or ‘somatic’ approaches to trauma therapy. “The body keeps the score” (2015), is Bessal Van Der Kolk’s seminal book as a world leading trauma therapist. It is also the field of research of Stephen Porges and Deb Dana (2018), whose book “Polyvagal Theory” explains how the body’s nervous system is shaped by our early attachment relationships. Their theory informs this blog as it explores the body-brain connection and explains the body’s nervous system response to childhood trauma. Finally, it is my hope this blog will allow you, the reader, to gently consider how your own body holds past relational trauma, to honor your body’s learned responses and find a pathway that leads to a kinder and more harmonious relationship to yourself, to your body and toward others.
Our Automatic Surveillance System within our Nervous System
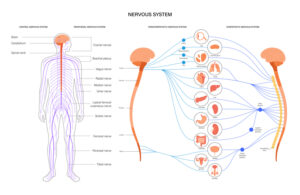
“We come into the world wired to connect. With our first breath, we embark on a lifelong quest to feel safe in our bodies, in our environments, and in our relationships with others” (Dana, 2018, pp. 7,8). Feeling safe allows our bodies to function optimally and be able to learn new skills. Understanding what it means to feel ‘safe’ in our bodies allows us to speak out when we don’t feel safe. This also puts the focus firmly on the body’s nervous system, where our automatic surveillance system is working under the ‘radar’ of conscious awareness to keep us safe. This involves two branches, the sympathetic and parasympathetic branches of the Autonomic Nervous System (ANS), which are constantly at work to ensure we survive in moments of danger and thrive in times of safety. This system connects our brain and our body, and operates by constantly scanning the environment, listening moment by moment to what’s happening within our bodies and in our connections to others, ready to initiate a response in aid of our survival (Dana, 2018, p. 8).
Our survival brain sends a response via one of three nerve pathways within the ANS: the sympathetic pathway, found in the middle part of the spinal cord, responds to danger, preparing us for action by triggering the release of adrenaline which fuels the fight/flight response; the other two pathways are found within the parasympathetic branch, travelling along the vagus nerve (meaning “wanderer”). From the brainstem, the vagus nerve travels in two directions: upward, the ventral vagal pathway connects with nerves in the neck, throat, eyes, and ears and responds when we feel safe and connected. The dorsal vagal pathway travels downward through the lungs, heart, diaphragm, and stomach and responds to cues of extreme danger by taking us out of connection, out of awareness, to a protective state of collapse, numbness, or ‘not present’. These automatic pathways working together are the basis to understanding “Polyvagal Theory” which describes how our autonomic nervous system is learning to respond and being shaped by our early experiences of safety and/or danger. This learning becomes the operational system that undergirds and shapes all our present connections with others (Dana, 2018, p. xvii).
The two branches of the nervous system, the sympathetic (SNS) and parasympathetic (PNS) are working together, co-regulating the body’s automatic responses of heartbeat, breathing and digestion. In a simplified analogy, the ventral vagal acts like the ‘brake’, slowing our heartrate and breathing. We ‘accelerate’ with energy from the sympathetic nervous system, which releases the vagal ‘brake’. In danger, the ‘accelerator’ of sympathetic energy with its fight/flight response is fully activated, discharging adrenaline and cortisol (Dana, 2018, pp. 28,29).
Using imagery, Dana (2018), described how these pathways working together provide us with the lived experience of ‘well-being’. Firstly, using the image of a house, she described how the dorsal vagal system in the background runs the “basic utilities” of the home, regulating the rhythms of heartbeat and breath. The home’s security system, the sympathetic branch triggers alarm to react to immediate emergencies; then returns to standby when we are safe. In safety, the ventral vagal system allows us to enjoy our home as a place of rest and renewal, and welcome family and friends (p. 14). Secondly, Dana used the image of a ladder to describe daily movements within the nervous system; from the top of the ladder, in ventral vagal, we can enjoy our home, feel rested and renewed and enjoy the space with family and friends. When we feel under threat, the security alarm, our fight/flight response triggers movement down the ladder where we are equipped with resources for emergencies. Finally, the dorsal vagal at the bottom of the ladder protectively shuts the house down but allows basic utilities to keep running. When we can move freely up and down this ladder, without being ‘stuck’ either in “fight/flight’ or ‘freeze’, “the integration of these systems allows us to be compassionate, curious about the world and emotionally and physically connected to the people around us” (Dana, 2018, p. 15).
Our Attachment Relationships shape our Nervous System’s Responses
These three pathways are working from early in utero, providing us with the foundation to how we experience the world. This means our childhood relationship history, particularly our nervous system’s responses within this environment provides foundational answers to how our nervous system responds today, and the clues to alleviate our suffering (Dana, 2018, pp. 4,7). Within our early attachment relationships our autonomic nervous system is learning about connection with others, shaping how we approach others, how we react to stress and how we learn. This happens via the innate ability of human brains and nervous systems to powerfully influence each other. This synchronizing of nervous systems between caregiver and infant is called “co-regulation”. The calm regulated state of the caregiver calms the child’s dysregulated state, creating resonance, and deepening safe connection and attachment. In the very apt description provided by Medina (2014), he wrote “Soil nurtures seed”. Within the soil of calm, safe and supportive relationships, where needs are met, emotions acknowledged, where we are seen, heard, and valued, we feel safe, and we have optimal conditions for growth. We also learn the self-regulating skills needed to calm our own nervous system to develop ‘healthy’ emotional and relationship skills. This process is also happening within adult relationships; where people around us are in a calm, regulated state (in ventral vagal activation), signals of safety are being sent and received and our physical, emotional, and psychological well-being improve when our nervous system is predominately operating within this social engagement system.
Because there are no perfect parents, all humans have experienced relationship rupture (or disconnection) as children and carry some degree of unprocessed trauma into adulthood. “Good-enough” parents are those with ‘enough’ self-regulating skills to repair ruptured relationships with their child which enables the child to build healthy “self” skills, and models vital relationship building skills, the precursor to healthy adult relationships.
How our nervous system is affected within unsafe Environments.
From infancy, the amygdala of the brain, that produces fear-based responses within the nervous system is fully mature and active, and proximity to parents is the key method that calms the infant’s fear response. The way in which caregivers protect and modulate their child’s fear becomes the model on which the child’s brain develops the ability to recognize and “down-regulate” their own fear response (Cozolino, 2010, p. 253). Because the brain’s fear-based neurobiology and pleasure and relational systems of the brain are linked, this directly affects the type of attachment the infant develops with their caregiver (Perry, 2017, p. 97). Johnson (2019), using Bowlby’s “Attachment Theory”, described how these attachment models or patterns of interaction are “encoded” in infants as mental models or protocols for responding within future relationships, and affecting partner choices (p. 7). These behaviors can be seen in repeated unsafe relationship choices and where adults find it difficult to leave an abusive relationship. Repeated attachment disruption, unreliable, inadequate, or unresponsive caregiving, all forms of mis-attunement to the infant’s needs, create an unsafe environment that also has many long-term effects on the child’s ability to cope with stress and learn from new experiences. It can result in longer term anxiety and adjustment disorders, impacting the child’s ability to live well, learn, and thrive. It also impacts their ability to read cues of safety and/or danger and react appropriately in these situations. Research findings showed that early deprivation or chronic stress increase the chance of damage to the brain, can affect memory and reality testing, and prolong the use of primitive defensive behaviors (Brown, Henning, & Wellman, 2005; Radley et al., 2006; Sapolsky, 1985) (Cozolino, 2010, p. 22).
Unsafe environments are most clearly seen where there is neglect, abandonment, emotional, physical and/or sexual abuse, all of which create defensive habits of survival, protection and/or shutdown within the child that protectively disconnects them from other people and from their own body’s responses and emotions. Children are ill-equipped to cope with calming their own nervous system, and fighting back or fleeing are maladaptive in an environment where their survival depends on caregivers. This creates an internal “shift” within the child’s nervous system, moving them down the ladder from the fear-based, hyperarousal system of “fight/flight” to the ‘protective’ state of “freeze”, which results in derealization and depersonalization reactions that allow the child to avoid the reality of what’s happening or watch it as a detached observer. These dissociated states create an internal environment that is disconnected from their own body’s responses and with internal boundaries that ‘block’ different emotional states and memories (Cozolino, 2010, pp. 269, 270).
When habits of survival and/or shutdown are reinforced, they become entrenched behavioral patterns which can be identified as mental health disorders. “Complex PTSD occurs in the context of early, prolonged, and inescapable trauma. It is called complex because of its extensive effects on all areas of physiology, development, and functioning” (Cozolino, 2010, p. 268). Johnson (2019) also connects mental health issues with an infant’s early relationships: “attachment insecurity increases vulnerability to the two problems most commonly addressed in therapy, namely depression and anxiety” (p. 11). Today, we are seeing an increasing prevalence of anxiety disorders, particularly among children, potentially caused by such factors as unsafe intrusions or bullying via social media and school, and increased stress in homes producing overwhelmed/anxious parents and anxious children (Cohen, 2013, p. xvi).
Furthermore, in an increasingly complex society, children who ‘don’t fit’ socially or have a different learning style, who can’t keep up with peers and feel alone in their struggles, the loneliness of social exclusion brings not only feelings of being unsafe, activating the danger defense system, it also brings emotional pain that activates the same pain pathways as experiences of injury and physical pain (Dana, 2018, p. 49). Children and/or adults from minority groups can have repeated experiences of social exclusion and/or bullying, all of which activate the body’s automatic defense systems. Where there is no support to resolve these issues, it makes safe connection even harder to access and creates further shutdown in the person and their sense of mastery in social situations. Pain induced defense patterns can lead to drug and alcohol addiction or other self-harming or anti-social behaviors that bring some immediate relief from pain, however, also bring further alienation, societal judgement, and mental health issues. The behaviors then become the focus, when in fact: “The PROBLEM is not the PROBLEM”.
Another extreme but helpful example of an overactive/maladjusted nervous system is provided by soldiers in wartime. Rigorous training is provided for recruits to condition their fight/flight reactions to be on ‘high alert’, prepared to function under the stress of combat conditions. However, this training does not allow them to process the intense emotions that accompany wartime experiences, nor does it prepare soldiers for re-entry into civilian life with their nervous systems trained to be on constant high alert and ready to react to any sound or trigger of threat. The painful aftermath of PTSD and/or self-harming behaviors including drug and alcohol overuse, all attempts by the soldier to calm their over-active nervous system wired for high alert, is the legacy of war for many returned servicemen.
In summary, from before birth our autonomic nervous system perceives cues from the world around us and from within our bodies, monitoring for safety and danger. Before our conscious ‘higher’ brain understands and makes meaning, the autonomic nervous system via the ‘lower’ brain regions has assessed the situation and initiated a response. Because we are shaped by our experiences, each person has their own response patterns, a result of the interplay of these two states … “We live in a story that originates in our autonomic state, is sent through autonomic pathways from the body to the brain and is then translated by the brain into beliefs that guide our daily living. The mind narrates what the nervous system knows. Story follows state” (Dana, 2018, p. 35). Our nervous system’s interpretation of the world is therefore the story of our lives. It is important to recognize and honor our nervous system for doing its job, to enable our survival through often difficult circumstances, even when we feel our body’s responses are out of our control and/or interfering with everyday functioning.
“Hopefulness lies in knowing that while early experiences shape the nervous system, ongoing experiences can reshape it” (Dana, 2018, p. 5). In the next blog I will explore how we can reshape our nervous system and develop the ‘tools’ needed to build safe relationships.
 Author: Lenore Hall, M. Couns, RN, B.Occ Th.
Author: Lenore Hall, M. Couns, RN, B.Occ Th.
Lenore is a Brisbane counsellor passionate about neuroscience, the impact of trauma, stress, and relationship on mental health, and the connectedness of physical, emotional, and spiritual well-being.
To make an appointment with Lenore please can call Vision Psychology Brisbane on (07) 3088 5422 or M1 Psychology Loganholme on (07) 3067 9129 or select here for Online Booking.
References:
Cohen, L.J., 2013, “The opposite of worry. The playful parenting approach to childhood anxieties and fears”
Cozolino Louis, 2010. “The Neuroscience of Psychotherapy”
Deb Dana, 2018. “The polyvagal theory in therapy”
Johnson, S., M., “Attachment theory in practice”.
Medina, J., 2014. “Brain rules for baby. How to raise a smart and happy child from zero to five”
Perry, P.D. & Szalavitz, M., 2017 “The boy who was raised as a dog.”
Van Der Kolk, B., 2015, “The body keeps the score.”